New Hope & Healing from Advanced Technology
Providence Little Company of Mary is investing heavily in leading-edge medical devices—from surgical robots to focused ultrasound—so patients can benefit from faster, safer, less invasive treatments.
- CategoryAdvertorials, Health
- Written byAnne M. Russell
- Photographed byShane O’Donnell
The devices that make medical miracles possible are evolving rapidly, as robotics and artificial intelligence advance daily. Providence Little Company of Mary is determined to stay in the lead through ongoing investment in breakthrough equipment.

Above: Chief surgeon James E. Camel, MD, in the operating suite with the new da Vinci 5 surgical robot
•••
“This equipment is an investment in patient care,” says Nate Mabry, Providence Little Company of Mary’s chief administrative officer. “It only makes the patient experience better when you have superior care delivered in a less invasive way.”
He notes that the advanced technology is also important for the well-being of caregivers. “It creates an environment where you’re helping advance patient care. The whole community feels the benefit.”
Three leading-edge technologies have just come online at the medical center for patients with life-disrupting or potentially fatal conditions:
1. A NEXT-GENERATION ROBOT FOR “GENTLER” SURGERIES
Providence Little Company of Mary chief of surgery and robotic general surgeon James E. Camel, MD, says that what he values most about the hospital’s investment in the newest surgical robot is the benefits it brings to patients. “As a doctor, I’m always the biggest advocate for the patient,” says Dr. Camel, “and I really appreciate the administration’s investment in the DV5.”
The multimillion-dollar da Vinci 5 robot—the only system of its kind in the South Bay—allows complex abdominal and thoracic surgeries to be minimally invasive, which means a faster recovery with less pain for the patient. The tiny surgical tools that the surgeon controls from a console allow greater precision with a more “delicate touch,” which can result in less tissue trauma. That in turn can lead to less time under anesthesia for the patient as well as less blood loss and scarring.
While used primarily for scheduled urological, gynecological, thoracic and general surgery procedures, the robot has the potential to be an asset in emergency surgeries as well, Dr. Camel notes. It also promises to allow easy and effective expert consultations during surgery, since it can link off-site physicians into what the lead surgeon is seeing and doing in real time.
“There are so many implications for this technology,” says Dr. Camel. “We’re seeing better outcomes and quicker recoveries in these minimally invasive procedures. Those are the things that change medicine.”
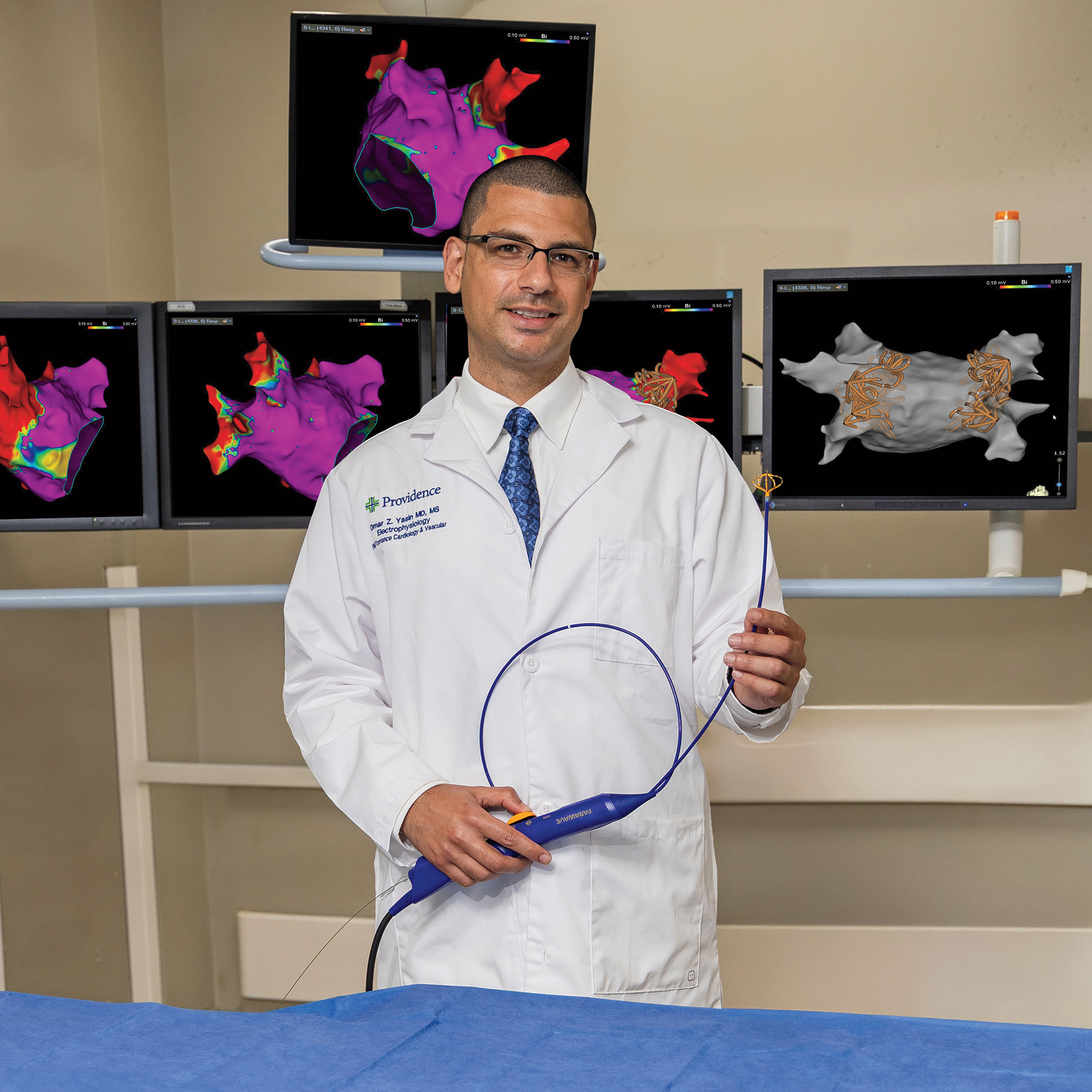
Cardiac electrophysiologist Omar Z. Yasin, MD, with the Farapulse PFA system that he uses to treat atrial fibrillation
2. PULSED FIELD ABLATION TO STOP ATRIAL FIBRILLATION
For the 7 million Americans who suffer from atrial fibrillation (A-fib), heart arrhythmia isn’t just an inconvenience or discomfort. It means they face a five times greater risk of a life-threatening stroke. When the two upper chambers (atria) of the heart beat irregularly, it can cause blood to pool and clot with the risk the clot will travel to the brain.
Until last year, the only surgical treatment option for A-fib was thermal ablation. During a thermal ablation procedure, a physician uses heat or cold delivered via a catheter threaded into the heart to destroy the tissue that’s producing the abnormal rhythm signal. While it’s usually effective in stopping A-fib, thermal ablation can inadvertently destroy surrounding tissue, such as the esophagus or phrenic nerve—sometimes with deadly consequences.
Pulsed field ablation (PFA) uses the same concept and similar methodology, but with more precision because the seconds-long pulse of energy is tuned to destroy only cardiac tissue with no spillover. Omar Yasin, MD, a cardiac electrophysiologist with Providence Little Company of Mary, is pleased with the new technology.
“This is better for patients,” he says. “It’s quicker and easier, and it’s allowed us to help a lot of patients who would not have tolerated thermal ablation.”
The Farapulse PFA system was approved by the U.S. Food and Drug Administration in early 2024. The procedure, Dr. Yasin says, allows many patients to forgo general anesthesia in favor of lighter sedation—a huge advantage for elderly or frail patients. And it hastens postsurgical recovery. Start to finish, PFA takes less than 2½ hours and is usually done as an outpatient treatment.

Above: Natalie Diaz, MD, and Jean-Philippe Langevin, MD, who specialize in treating movement disorders, with the new focused ultrasound system
•••
3. FOCUSED ULTRASOUND TO END ESSENTIAL TREMOR
Essential tremor is by far the most common movement disorder, affecting about 10 million Americans. It is called “essential” because it stands on its own—it’s not caused by any other disease or condition, unlike the shaking due to Parkinson’s disease.
Essential tremor usually starts in the hands, but the tremors can also involve the face, head, neck and even the voice. And while the condition itself isn’t life-threatening, the depression and isolation that might result when it becomes severe can be.
For many patients, pharmaceutical options either don’t control the tremors or cause intolerable side effects. So until recently, that left only one option: brain surgery. The procedure, which has a 20-year track record, is known as deep brain stimulation (DBS) and involves implanting electrodes in the brain that receive electrical bursts from an implantable pulse generator in the chest to disrupt the brain’s erroneous signals.
Now there’s a new, much less invasive possibility: focused ultrasound. Providence Little Company of Mary is the only South Bay hospital to offer it. Both Natalie Diaz, MD, a neurologist specializing in movement disorders at the Pacific Neuroscience Institute at Providence Little Company of Mary, and Jean-Philippe Langevin, MD, a neurosurgeon specializing in movement disorders who is also the director of the Restorative Neurosurgery and Deep Brain Stimulation program at the institute, say they are excited about the promise of the new system.
It’s an especially attractive alternative for patients taking blood thinners because, unlike DBS, focused ultrasound doesn’t require that they stop taking anticoagulant medications. “Focused ultrasound represents a superior option,” says Dr. Langevin.
The procedure takes about 2½ hours and focuses ultrasound energy on a pinpoint-sized spot in the brain to destroy the tissue causing the tremor. “This is a game changer,” Dr. Diaz adds. “It’s a less invasive option. There’s no cutting. There’s no anesthesia. There’s no hospital stay.”
Mabry notes that keeping up with the most advanced equipment isn’t just about delivering superior patient care. It is also about offering an optimal workplace to hospital professionals.
“The doctors and nurses know that they’re doing important work that’s not being done in other places. They’re helping advance medicine,” he says. In turn, “The patients reap the benefits of having highly engaged caregivers.”